August-2020 Type-A Dissection - Emergent Surgery
In August-2020, the Foundation’s Benefactor suffered a Type-A Aortic Dissection resulting in pre- and intra-operative cardiac arrest requiring acute resuscitation measures. The Lead First Assist and CT Physician Assistant (also a tenured professor in the department of surgery) presented the case at APP Grand Rounds.
Our benefactor received external cardiopulmonary resuscitation during prep and open cardiac massage during the procedure. The lack of regular perfusion to critical organs during this time resulted in some permanent anoxic brain injury. Although he was able to recover much of these deficits through grueling physical and psychological therapy, he does have lingering effects.
These lingering effects, including malperfusion of his bowel / small intestines has resulted in the need for operative disimpactions where ‘obstructed fecal matter’ must be manually evacuated through operative means to enable relief to his distended abdomen. These procedures are done under local anesthesia and are incredibly painful.
His upcoming surgery (Open TAAA with AEF repair - described below) was taken on under the condition that it would be a ‘teaching case’ due to the incredibly high on-table mortality rate.
UPCOMING SURGERY:
Benefactor is scheduled for an Open TAAA repair with repair of an Aortoesophageal Fistula (AEF). He will be working with a professional advocated to help him prepare for this marathon surgery that carries an ‘on-table’ mortality risk of up to 70%.
Open Thoracoabdominal Aortic Aneurysm (TAAA) Repair - The ‘Mother of all Aortic Surgeries’
Open Thoracoabdominal Aortic Aneurysm (TAAA) repair is the most high-risk cardiovascular surgery performed today - especially for those with connective tissue disorders like Marfan Syndrome (“MFS”) that have the Type II variant, which is the most extensive in terms of amount of diseased aortic tissue involved. The primary risks associated with thoracoabdominal aortic aneurysm (TAAA) repair-namely operative death, paraplegia, and renal failure necessitating dialysis-are commonly related to the distal ischemia that occurs during aortic clamping and the disruption of vital branching arteries.
The technique for open TAAA repair has evolved over the course of 3 decades, from the unheparinized, simple "clamp-and-sew" approach learned directly from E. Stanley Crawford himself to a contemporary, multimodal strategy that uses an array of surgical adjuncts. Today, the approach to TAAA repair is largely standardized and based on the Crawford extents of TAAA repair, but we have maintained flexibility to explore new techniques and to adapt to the specific needs of patients. To protect the spinal cord, the surgical team routinely uses mild passive hypothermia, cerebrospinal fluid drainage, left heart bypass, and reimplantation of crucial intercostal or lumbar arteries. The renal arteries are perfused with cold solution to protect the kidneys from ischemic damage, and the celiac axis and superior mesenteric artery are perfused with isothermic blood from the left heart bypass circuit, which minimizes the duration of abdominal-organ ischemia.
The most extensive repair, Crawford extent II repair, typically replaces the aorta from just beyond the left subclavian artery to the aortic bifurcation; unsurprisingly, it commonly poses greater operative risk than do less extensive TAAA repairs (extent I, III, and IV). Subsequently, most surgical adjuncts used today were developed to ameliorate risk in extent II repair. Here, we provide a detailed description of our approach to open extent II TAAA repair.
**Open TAAA repair used to carry very high operative mortality rates and significant risk of paraplegia (if the patient survived surgery). Today, at Aortic Centers of Excellence with high volumes of Open TAAA repairs, this remains a daunting and barbaric surgery (often lasting many hours) fraught with complications. Most patients will not qualify for Open TAAA repair due to co-morbidities.

Patient positioning - lateral decubitus position.

Prepping the patient's entire torso for surgery (neck to toes)

Incision for Extent II TAAA repair goes from upper scapula all the way across the front of the abdomen down to the pubis.
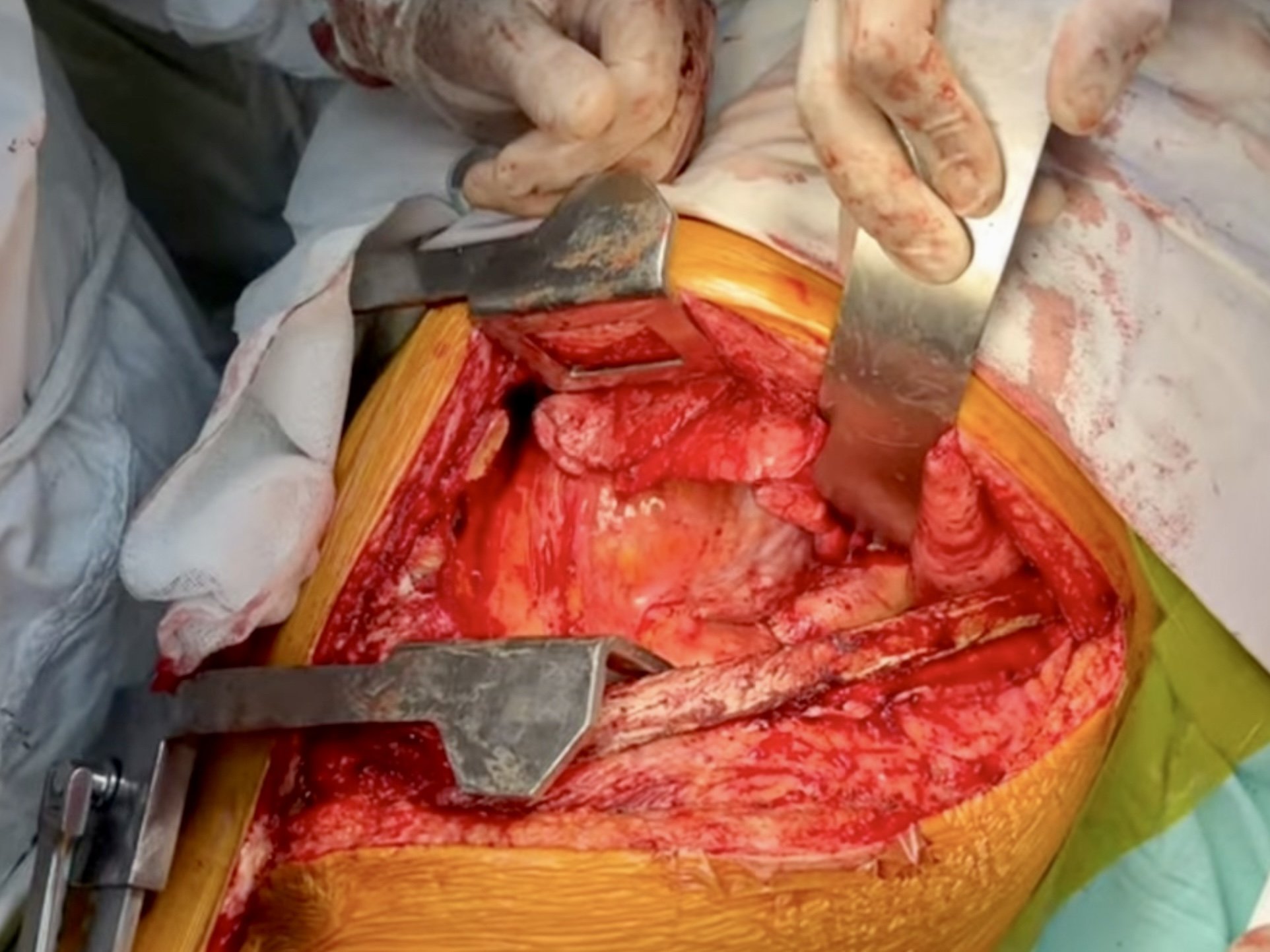
Cracking the patient open for adequate exposure using self-retaining retractors.

Intense point of operation with team attempting to establish control of all the clamps in the massive surgical field.

Patient 'cracked-in-half' so surgical team can begin work on replacing the diseased aorta with dacron grafts.

Closing the chest wall with thick-gauge needles. Post-operative pain has been described as unbearable.

